
Sleep Apnea and Snoring: Why You Wake Up Tired
Medically reviewed by Patricia Weiser, PharmD and Jared Meacham, PhD, RD, CSCS
Getting enough good quality sleep can be challenging in the face of everyday stress and busy schedules. It’s even more challenging if you have the sleep-related disorder sleep apnea or if you snore without this condition. Sleep apnea and, to a lesser extent, snoring prevent your body and brain from achieving optimal recovery. They can ratchet up your stress response, leaving you exhausted the next day. Sleep apnea can also put your health at risk. But both sleep apnea and snoring are treatable, and treatment can help you unlock better sleep.
Does this sound familiar? You go to bed and at night and wake up at the same time each morning, sticking to a solid sleep routine. You ensure you log more than seven hours of slumber on most nights. Yet you’re groggy in the mornings and find fatigue creeping up on you throughout the day. What gives?
If this is you, sleep apnea, snoring, or both might be getting in the way of your zzzz’s. Sleep apnea is a disorder that causes periods where you temporarily stop breathing while sleeping. It most commonly happens when the throat muscles relax too much, causing the airway to collapse and block airflow.
Most people with sleep apnea also snore, but not always. And snoring can also occur on its own without sleep apnea. Both sleep apnea and snoring can leave you feeling like you barely slept the night before.
In this article, we explore what sleep apnea is, what causes snoring, whether snoring means you have sleep apnea, how to tell if you snore or have sleep apnea, how to reduce snoring not related to sleep apnea, and how to improve your rest with BetterSleep.
Sleep Apnea and Snoring: What’s the Connection?
“Snoring and sleep apnea are part of a spectrum,” says Daniel Slaughter, MD, a sleep medicine and ear, nose, and throat (ENT) expert at Sinus & Snoring Specialists.
Airflow resistance during sleep that does not involve episodes of airway collapse or periods where breathing starts and stops is called primary snoring, simple snoring, or non-apneic snoring. It’s a type of sleep-related breathing disorder (SRBD).
“[Snoring] disrupts the bed partner and may also lead to poor quality sleep for the patient,” Dr. Slaughter adds.
Newer preliminary research suggests that snoring may also impact health in some ways beyond how well you sleep, but more studies are needed to confirm. Mild snoring without airway issues or sleep disruption is generally harmless, while heavy snoring often signals sleep apnea.
Sleep apnea is a sleep disorder that occurs when you stop and start breathing many times throughout the night. This leads to poor sleep quality, often resulting in next-day sleepiness.
But the issue goes beyond feeling tired, which can be dangerous while driving or operating machinery and may impede your focus while doing work or everyday tasks.
Untreated sleep apnea can be deadly, and it puts you at risk for several chronic conditions, including:
- Congestive heart failure
- Dementia
- Heart attack
- High blood pressure
- Heart arrhythmias (irregular heart rhythms)
- Kidney issues
- Obesity
- Liver issues
- Metabolic syndrome
- Prediabetes and type 2 diabetes
- Stroke
Proper treatment, however, helps maintain breathing during the night, reducing risk for complications. Treatment will depend on the type of sleep apnea you have. The types are listed below. For certain adults with obesity and sleep apnea, a prescription medication (tirzepatide) may be beneficial. However, treatment for all types commonly includes the use of a continuous positive airway pressure (CPAP) machine. Sometimes surgery is also an option. Additionally, some oral appliances that help reposition the jaw or stabilize the tongue may be appropriate.
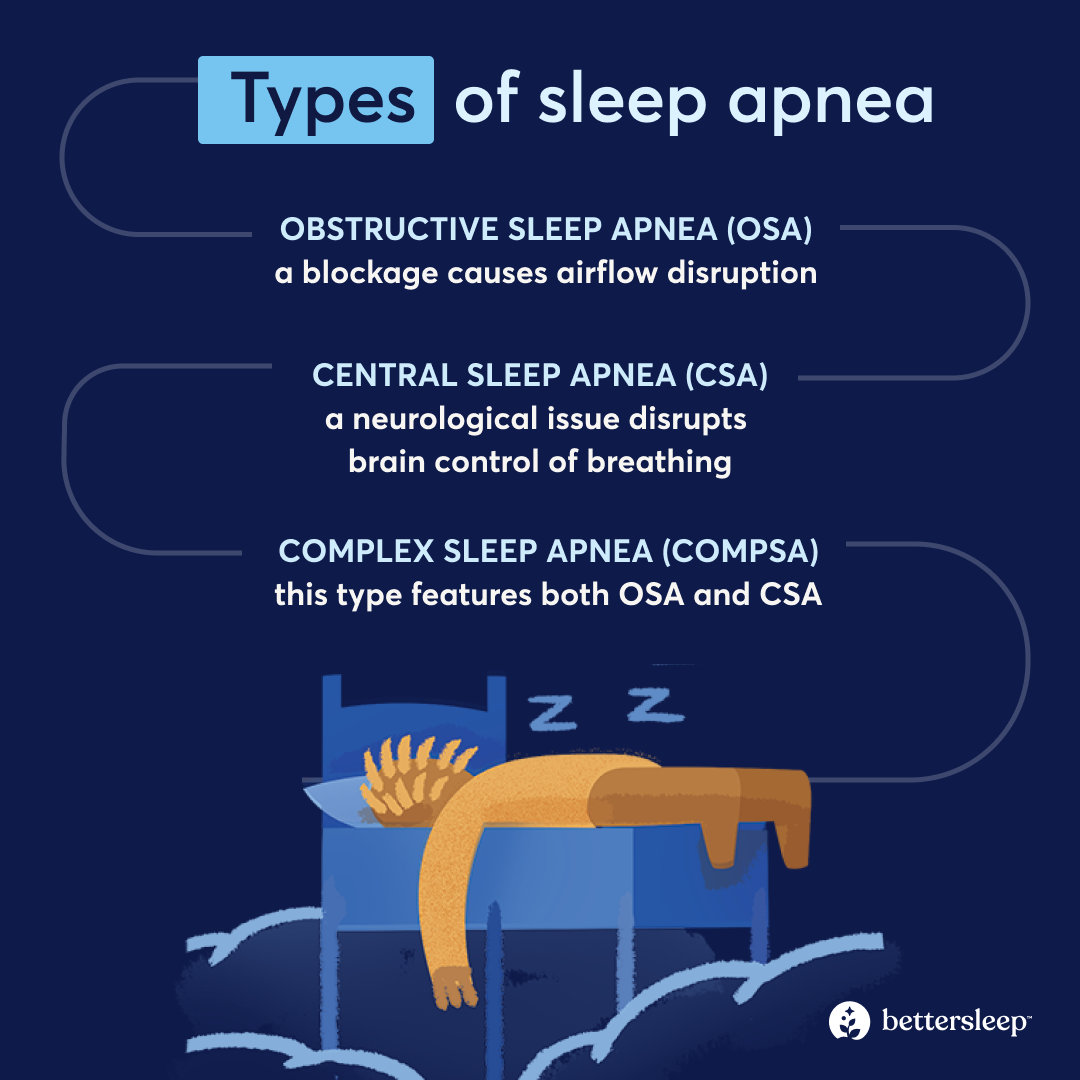
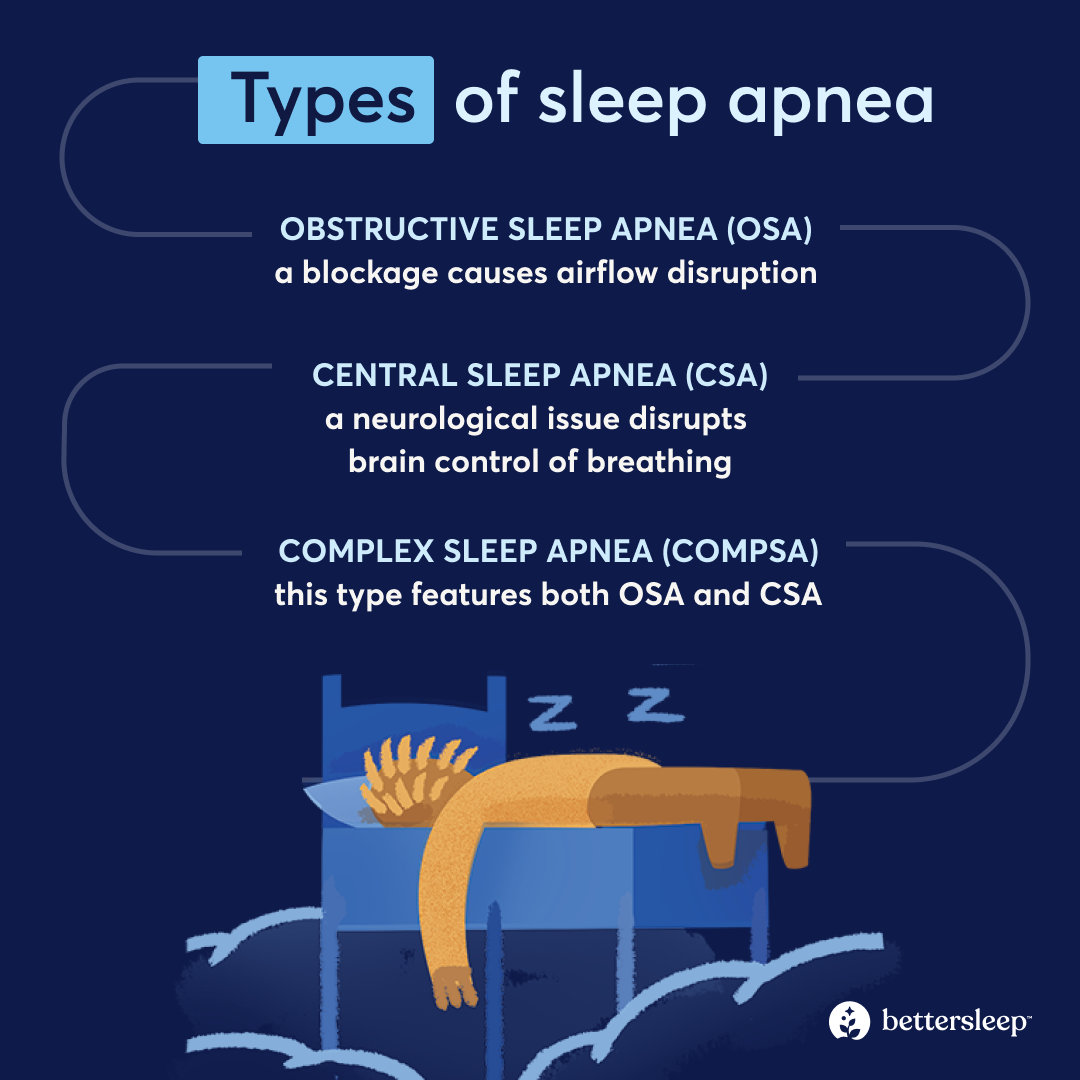
Types of sleep apnea
- Obstructive sleep apnea (OSA): A blockage causes airflow disruption due to a partial or complete collapse of your upper airway. OSA is the most common type of sleep apnea.
- Central sleep apnea (CSA): A neurological issue disrupts communication between the brain and muscles that control breathing.
- Complex sleep apnea (CompSA): This type features both OSA and CSA.
Snoring Causes: What’s Actually Making the Noise?
“Snoring occurs when the airway partially collapses and tissues vibrate as air passes through,” says Madan Kandula, MD, an ENT and CEO of ADVENT.
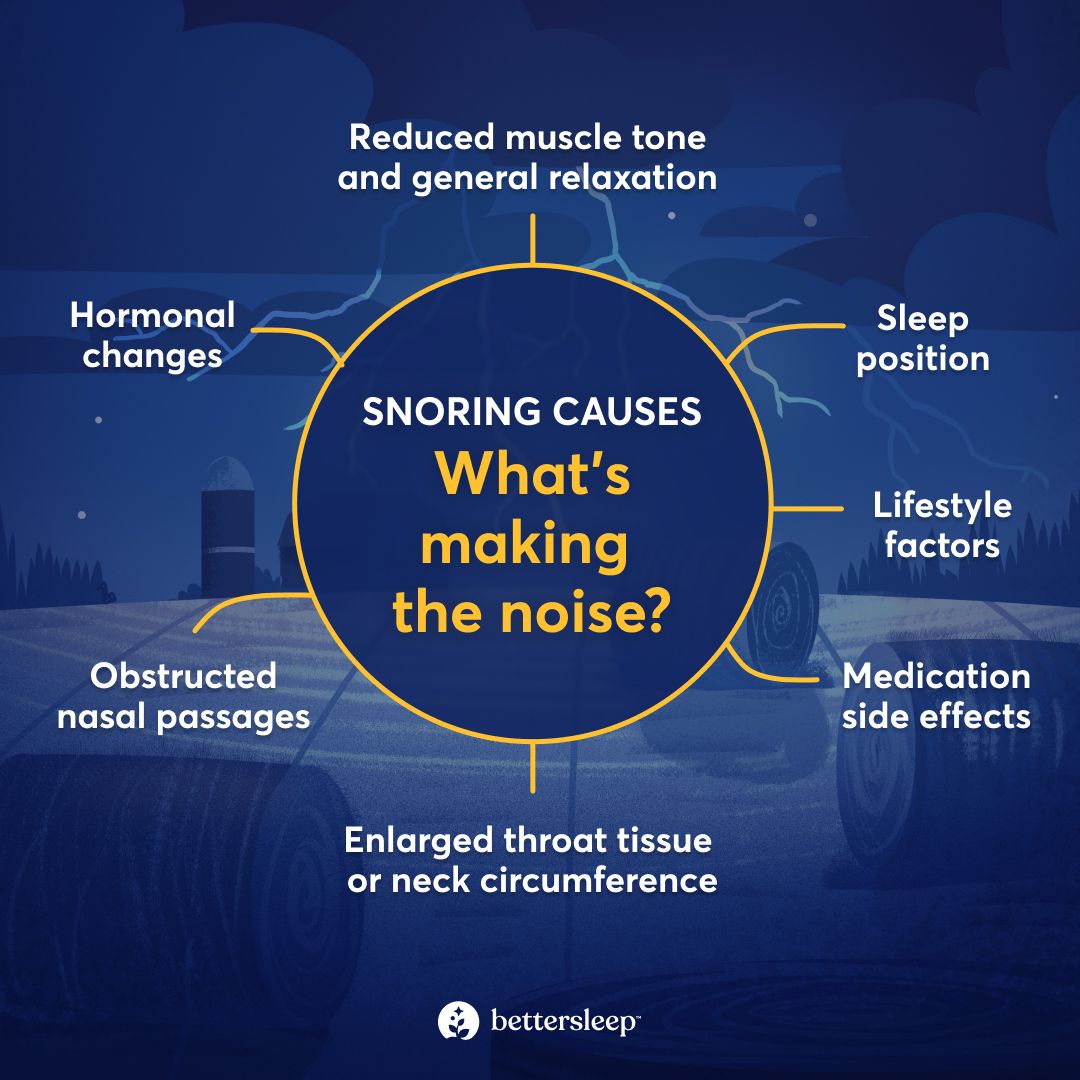
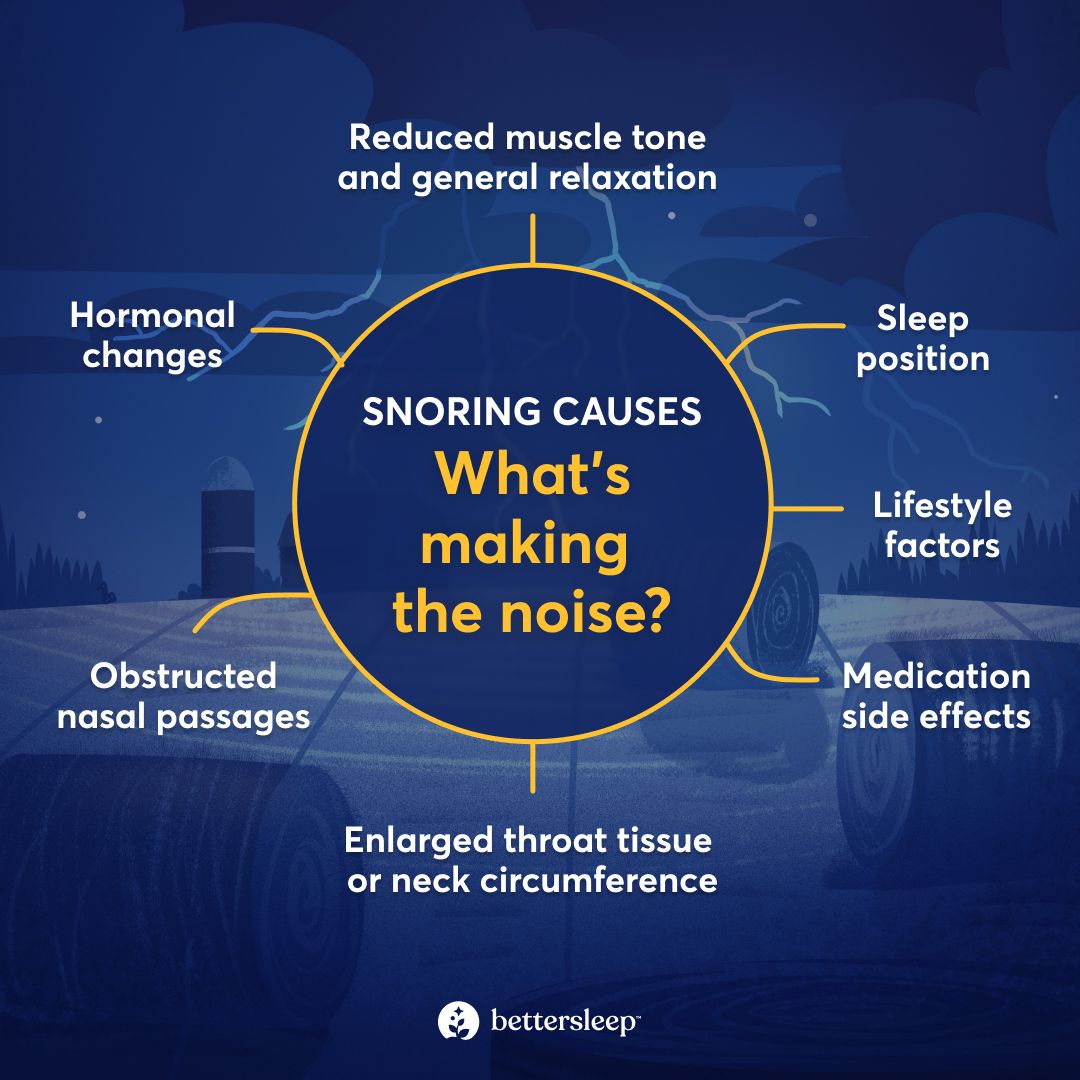
With primary snoring, meaning snoring not attributed to sleep apnea, the causes run the gamut.
- Enlarged throat tissue or neck circumference: Throat structures, including adenoids and tonsils, can become inflamed or enlarged, obstructing airflow. Additionally, obesity or genetics can factor into neck size. A larger neck circumference—defined as 17 or more inches for males and 16 or more for females—increases snoring risk.
- Hormonal changes: For females, snoring and OSA are more common after menopause, when estrogen and progesterone have declined. And for males, OSA is more common in those who have a testosterone deficiency, which can occur as a natural part of aging or from other factors.
- Lifestyle factors: Alcohol consumption depresses the central nervous system. And smoking damages cilia, minuscule hair-like structures in the respiratory system that help filter and clean airways. Both drinking and smoking can trigger snoring in people who normally don’t have the issue or worsen it in people who regularly snore.
- Medication side effects: Some medications are linked to airway collapse or affect breathing, leading to snoring episodes. These include:
- Anticonvulsants
- Antidepressants
- Antipsychotics
- Benzodiazepines
- Muscle relaxants
- Opioids
- Sedatives and hypnotics
- Testosterone therapy
- Obstructed nasal passages: Structural issues can cause snoring—including a deviated septum (when the cartilage that separates your nostrils is misaligned) or enlarged or inflamed turbinates (bony nasal protrusions that help filter air). Additionally, a stuffy nose from illness, allergies, pollution exposure, and more can also impede airflow or lead to mouth breathing, triggering nighttime noises.
- Reduced muscle tone and general relaxation: Over the course of your sleep session, your muscle tone changes. During deeper sleep states, your muscles relax significantly. You might also lose muscle tone in your airway structures as you age, increasing your risk for snoring.
- Sleep position: Your sleep position can make gravity more potent on your soft airway tissues and tongue. In studies looking at OSA, snoring most often occurs when people sleep on their back. Stomach sleeping can also trigger snoring. You’re least likely to snore while sleeping on your side. But even then, snoring can ensue.
Does Snoring Mean Sleep Apnea? How to Think About Risk
“Snoring is often sleep apnea’s calling card,” Dr. Kandula says. “It signals restricted airflow during sleep. Not everyone who snores has sleep apnea, but nearly everyone with obstructive sleep apnea snores at some point.”
As Dr. Kandula notes, sleep apnea and snoring can each show up on their own, so snoring does not always mean you or a loved one has sleep apnea, but it can be a sign.
“Because of this overlap,” he adds, “habitual or loud snoring should be evaluated to rule out airway obstruction and sleep apnea.”
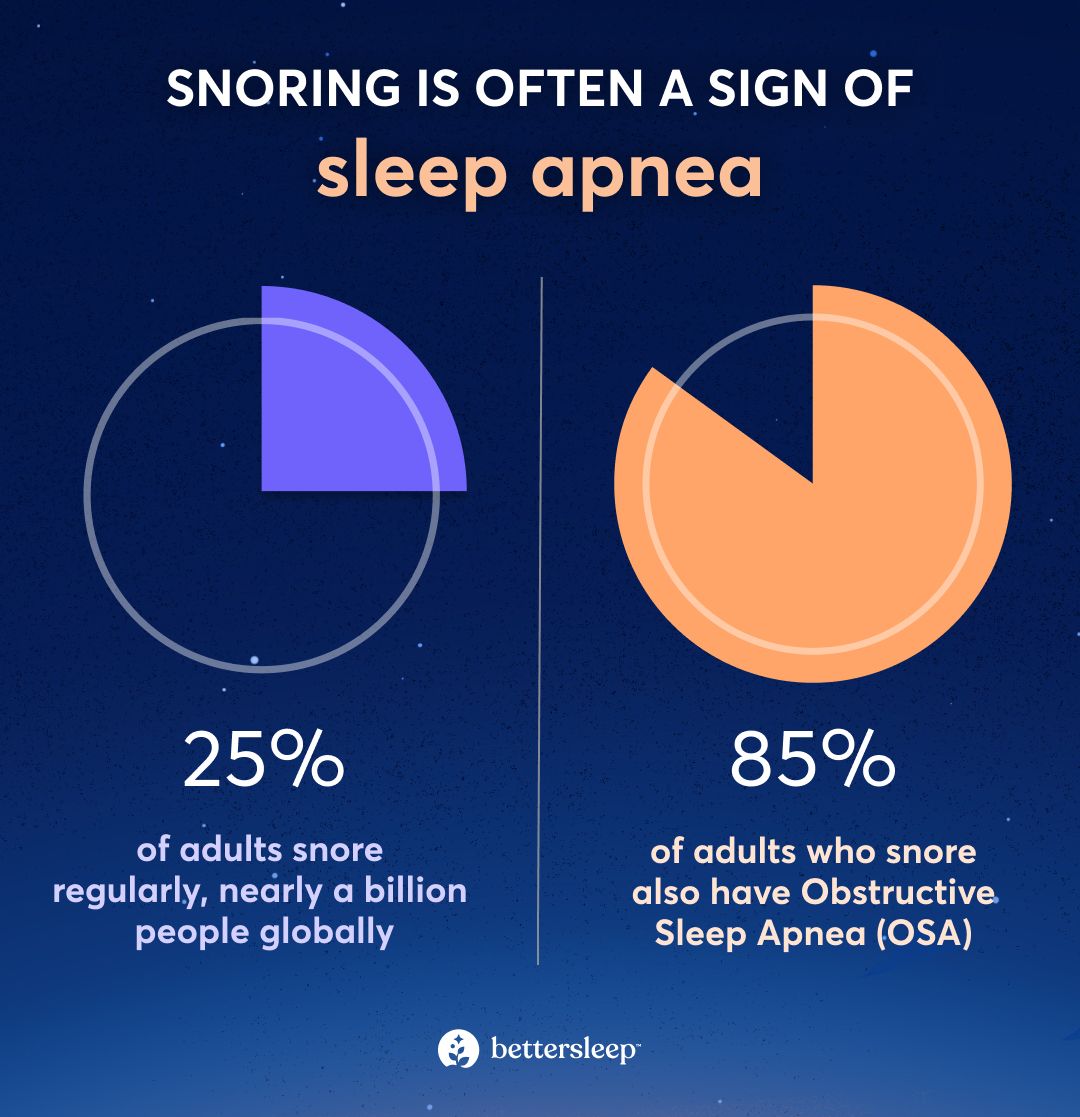
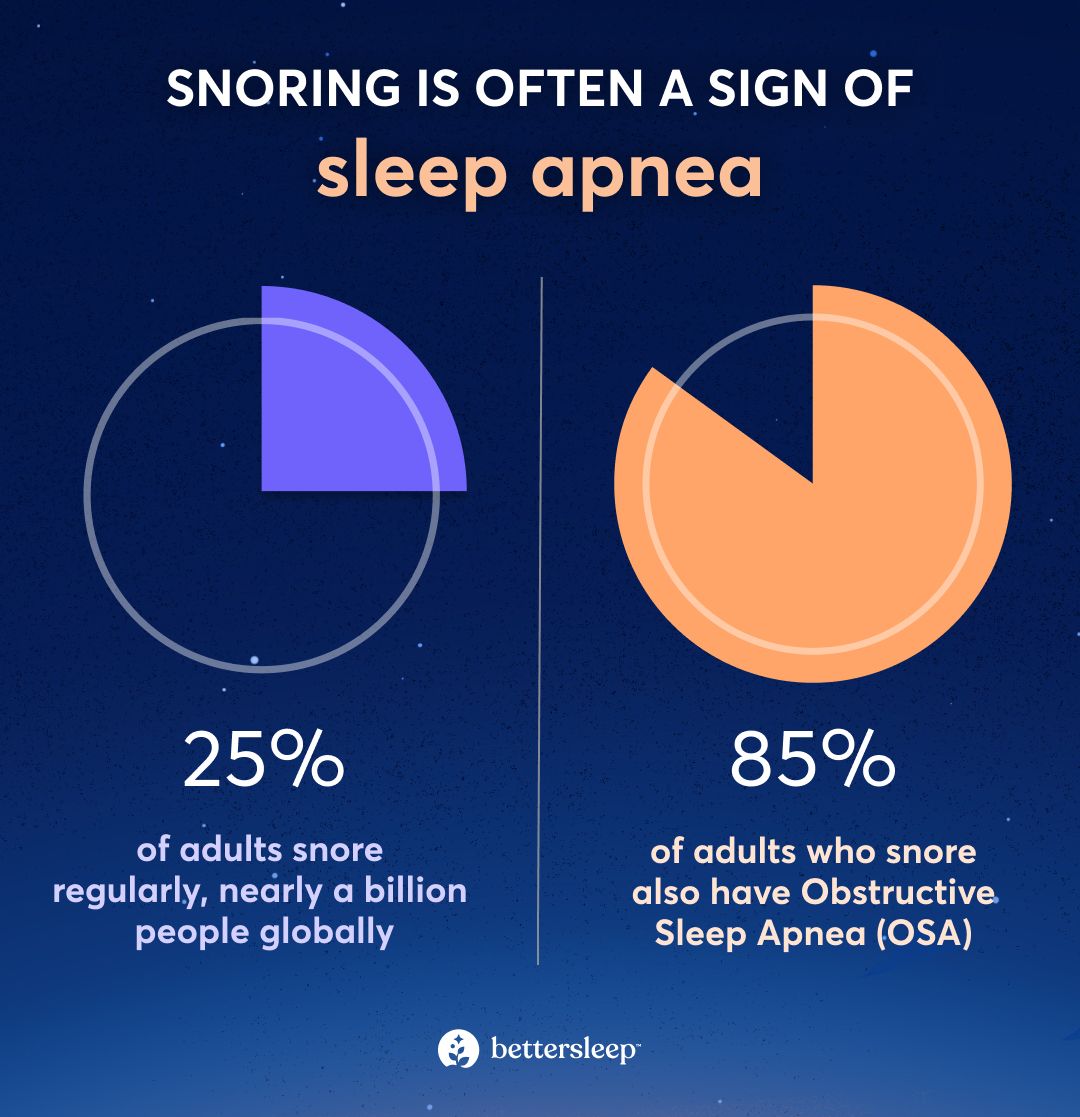
Almost half of adults snore at least some of the time. About a quarter do so regularly. Meanwhile, sleep apnea affects about 40 million people in the United States (more than 11% of the population) and nearly a billion people globally.
Research suggests that more than 85% of people with OSA also snore. However, snoring is much less common in people with CSA and is not a prominent feature of this type. People with CompSA may or may not snore.
Signs You Stop Breathing While Sleeping
“How do I know if I have sleep apnea?” If you’re asking yourself this question, you can review the symptom list below. If you do have symptoms consistent with sleep apnea, seeing a clinician is crucial.
“After a consultation with your physician,” Dr. Slaughter says, “if they suspect OSA they will typically order a sleep study. This is the definitive test to make the diagnosis.”
Dr. Kandula adds that a sleep study “measures breathing, oxygen levels, heart rate, and sleep quality over night.”
If you share your bed with a partner, they can be instrumental in keeping an eye out for some symptoms that occur while you sleep. You can also use your phone to record yourself to see if you snore, stop breathing, or gasp for air. Give the BetterSleep Sleep Recorder a try.
Just because you have one or more of these symptoms doesn’t mean you automatically have sleep apnea. Ultimately, the only way to know is to get evaluated by a physician.
Sleep-related symptoms:
- Breathing pauses
- Breathing that is shallow or irregular
- Bruxism (grinding teeth)
- Dry mouth or sore throat upon waking
- Frequent wakeups
- Frequently having to use the bathroom
- Insomnia
- Restlessness or excessive movement
- Night sweats
- Snoring
- Snorting, gasping, choking, or coughing
Daytime symptoms (or those noticed when awake):
- Chest pain or discomfort
- Fatigue
- Grogginess upon waking after adequate sleep
- Headaches upon waking
- Heart palpitations or irregular heart beats
- Microsleeps (falling asleep briefly and unintentionally during the day)
- Shortness of breath
- Sleepiness
- Swelling in ankles or legs
Mental health and cognitive symptoms:
- Anxiety
- Amotivation (feeling a lack of drive to do tasks or favorite activities)
- Depression
- Irritability
- Mood swings
- Social withdrawal
Why You Wake Up Tired
“Sleep apnea causes repeated breathing interruptions and drops in oxygen throughout the night,” Dr. Kandula explains. “Each event forces the brain out of deeper, restorative sleep, even if the person doesn’t fully wake up.”
Restricted airflow forces the body to work harder to breathe. “This constant sleep fragmentation prevents full recovery,” he adds, “leading to unrefreshing sleep, daytime fatigue, and reduced alertness.”
Additionally, sleep apnea activates your sympathetic nervous system, (your “fight-or-flight” response). These activations cause stress to your body and brain and can lead to increases in cortisol, “the stress hormone.” Constant activation of fight-or-flight mode hinders your ability to adapt to daytime stress, to relax and unwind even when exhausted, and to regulate your emotions. All these factors can leave you feeling wired but tired.
Does primary snoring (without sleep apnea) lead to the same or similar issues? If snoring wakes you up or causes restlessness, then yes, the potential is there. You might have a condition called upper airway resistance syndrome. This is the “middle ground” on the continuum of simple snoring and OSA.
Snoring Relief You Can Try Tonight
If you suspect you have sleep apnea, be sure to get evaluated by a doctor. However, if you are looking for snoring relief you can try immediately or in the short term, here are a few tips. These are also great tactics to try if you learn from your physician that you have primary snoring without sleep apnea.
- Avoid alcohol and tobacco: If you don’t drink or smoke, skip taking up these habits. If you do like the occasional beverage, avoid consuming too close to bedtime and keep the number of drinks to a minimum. If you smoke or vape, talk to your doctor about a way to quit that makes sense for you.
- Change your sleep position: If you’re a back or stomach sleeper, try sleeping on your side. But if you prefer sleeping on your back, then elevating your head and torso slightly, with extra pillows, a wedge pillow, or even an adjustable bed base may help.
- Keep nasal passages open: If you have nasal congestion from an illness, treating with an over-the-counter decongestant may open your airways, though talk to your doctor to ensure you’re cleared to take one of these meds. If allergies plague you, mitigate your triggers, such as dust mites, and take prescribed medications as directed.
- Manage weight: If you have obesity, a chronic condition, reducing weight may decrease snoring. Weight management is complicated because of complex hormonal mechanisms. Talk to your doctor if you’ve tried lifestyle changes. You may need medications or other treatment methods to support your diet and exercise efforts.
- Stick to a solid sleep routine: Going to bed and waking up at the same times each night and day can help improve your quality of sleep and overall health. If you need a good wind-down routine, the BetterSleep app can help with soothing sounds, white or pink noise, guided meditation, and more.
The Bottom Line
Snoring sometimes serves as a clue that you have sleep apnea, a serious condition in which you stop and start breathing several times throughout the night. However, snoring and sleep apnea can occur independently of each other. Either way, both can lead to next day sleepiness, general fatigue, irritability, and health issues.
The good news is that both sleep apnea and primary snoring are treatable conditions. The crucial step is to talk to your doctor for an evaluation and any necessary treatment and to prioritize good-quality sleep by crafting a sleep routine that fits your needs. BetterSleep is here to help.
Key Takeaways
- Snoring and sleep apnea sometimes go hand in hand, though they can each occur independently.
- Both conditions can leave you tired the next day, even after logging a full night’s sleep.
- Untreated sleep apnea can also lead to significant health issues, so if you suspect you have it, talk to your doctor asap.
- Some at-home changes can help alleviate snoring not caused by sleep apnea. And the BetterSleep app can help you improve your overall sleep so you wake up feeling rested.
Frequently Asked Questions (FAQs)
What is the 3% rule for sleep apnea?
The 3% rule for sleep apnea is a scoring guideline used in sleep studies to diagnose the condition. It is not meant for self-diagnosis. During a sleep study, if your airflow drops by 30% for 10 seconds or longer and if your blood oxygen level drops by 3% or more, you will potentially be diagnosed with sleep apnea.
What are four symptoms of sleep apnea?
Four common symptoms of sleep apnea include snoring, periods where you stop and start breathing again throughout the night or sleep session, next-day sleepiness, and an inability to focus. These are not the only symptoms of sleep apnea, but they represent some classic signs.
How to know if it's snoring or sleep apnea?
The only way to know if you have sleep apnea, a serious medical condition, is to get evaluated by a physician and undergo a sleep study.






















