What is Sleep Paralysis? Science-Backed Guide to Causes & Solutions
Have you ever woken up unable to move, feeling like something’s pressing on your chest? That’s sleep paralysis—a surprisingly common but harmless glitch in your sleep cycle. Learn what’s really happening, why it feels so real, and how to prevent future episodes for calmer, more restful nights.
You open your eyes and realize you’re awake—but your body won’t budge. Maybe there’s a weight on your chest or a shadow at the edge of the bed. Your mind races, convinced something’s wrong. And then, just as quickly, it’s over. You can move again. Your heartbeat slows, but the fear lingers.
If that sounds familiar, you’re not alone. Sleep paralysis affects millions of people worldwide, and while it can feel terrifying, it’s completely harmless. It’s a short-lived disconnect between the mind and body during REM sleep—the stage where your brain is most active and dreams are vivid. For a moment, your body’s still “asleep” while your mind wakes up, causing the feeling of paralysis.
Because episodes can feel so real, they often leave a lasting sense of fear or confusion. But understanding what’s happening—and why—can take away much of that anxiety. Once you know the science behind it, sleep paralysis becomes something you can manage rather than something that controls you.
In this guide, you’ll learn how to:
- Understand what sleep paralysis is and why it happens
- Recognize common symptoms and sensations
- Stop an episode while it’s happening
- Prevent future ones through simple habits and better rest
- Know when to seek help from a sleep specialist
You’ll also find guidance from leading sleep experts and discover how BetterSleep’s sleep disorder resources can help you track patterns, manage stress, and create a calmer bedtime routine.
Sleep paralysis might feel overwhelming, but with right knowledge, reassurance, and a few small changes, peaceful nights are absolutely within reach.
What is Sleep Paralysis? Understanding the Phenomenon
Sleep paralysis is a temporary state where the body and mind fall slightly out of sync during the transition between sleep and wakefulness. For a short period—usually seconds, though sometimes longer—you’re awake and aware, yet unable to move or speak. The experience can feel as if your body has frozen while your thoughts remain fully alive. For many, that mismatch is terrifying the first time it happens.
The good news is that science understands this phenomenon well, and it’s both harmless and common. By understanding the brain and body’s role during these moments, the fear can ease.
The science behind it
During a normal night’s sleep, the body cycles through various stages, including rapid eye movement (REM). This is when most dreaming occurs and when the brain sends signals that quiet the body’s muscles so you don’t physically act out your dreams. Typically, these systems switch on and off together. In sleep paralysis, awareness comes back before muscle control does, leaving you alert but temporarily unable to move.
Researchers classify sleep paralysis as a type of parasomnia—a sleep disorder that occurs during transitions between wakefulness and sleep. Episodes usually last from a few seconds to two minutes. While anyone can experience them, some people are more prone than others due to stress, irregular sleep, or other underlying conditions.
Types of sleep paralysis
Experts generally describe two forms:
- Isolated sleep paralysis – single or occasional episodes unrelated to another medical condition
- Recurrent isolated sleep paralysis – episodes that occur repeatedly over time, sometimes linked to poor sleep, high stress, or inconsistent schedules
In both cases, the event itself is not dangerous. The distress often stems from the vivid awareness of being awake without control over movement or speech.
How common is it


Sleep paralysis is far more widespread than most people realize. Studies have shown that roughly 8 percent of the global population experiences at least one episode in their lifetime. The rate jumps to 28 percent among students and 32 percent among people with psychiatric conditions such as anxiety or depression.
Episodes can begin at any age but are most frequent in the late-teens through early thirties—a period when sleep patterns often fluctuate. Both men and women experience it, though some studies suggest a slightly higher prevalence among women.
Why it happens
Sleep paralysis doesn’t have a single cause; it actually results from a combination of biological, environmental, and lifestyle factors. Anything that disrupts healthy sleep patterns—work, chronic stress, anxiety, trauma, or inconsistent bedtimes—can increase risk. Essentially, the body’s timing gets off: the brain wakes up before the muscles have exited their dream-state stillness.
Genetics may also play a role. Twin studies suggest a hereditary component, though genes appear to interact with stress and sleep-quality factors rather than determining risk on their own.
Medical conditions that fragment sleep—such as narcolepsy, insomnia, or untreated sleep apnea—can make episodes more likely. For others, stimulants, certain antidepressants, or even sleeping on your back can be triggers.
The brain’s role
Neuroscientists describe sleep paralysis as a hybrid state of consciousness. Brain-imaging research shows that regions involved in alertness and perception (like the parietal and prefrontal cortices) activate, while other regions remain in REM mode. This overlap allows dream-like sensations—visuals, sounds, feelings of weight or presence—to blend with waking awareness. Because the mind is alert but the body is immobile, those sensations feel external and real.
Dr. Baland Jalal of Harvard Medical School explains:
"Sleep paralysis, while frightening, is a benign condition that poses no direct physical danger to those who experience it. Understanding the neurobiological mechanisms behind these episodes can significantly reduce the fear and anxiety that often perpetuate the condition."
This framing is key: fear and anxiety can actually increase future occurrences. Knowing the science can help break that cycle.
When to seek help
An occasional episode doesn’t usually require medical attention. However, if episodes are frequent or extremely distressing, they may indicate an underlying sleep disorder or mental health condition that warrants care. It’s worth consulting a sleep specialist if:
- Episodes occur more than once a month
- You experience severe anxiety or sleep avoidance afterward
- You also suffer from excessive daytime sleepiness or sudden loss of muscle tone
A clinician may recommend a sleep study to rule out narcolepsy, sleep apnea, or other disturbances that fragment REM. Treatment often focuses on improving sleep consistency and managing stress—simple changes that can make a major difference.
The bottom line
Sleep paralysis may feel supernatural, but it’s a normal variation of REM physiology. Your brain has a safety mechanism to prevent you from acting out your dreams, and sometimes that system lingers a little too long. Once you understand that, the fear often fades.
Knowledge turns the experience from something alarming into something explainable—and, more importantly, manageable.
Symptoms and Experiences: What Sleep Paralysis Feels Like
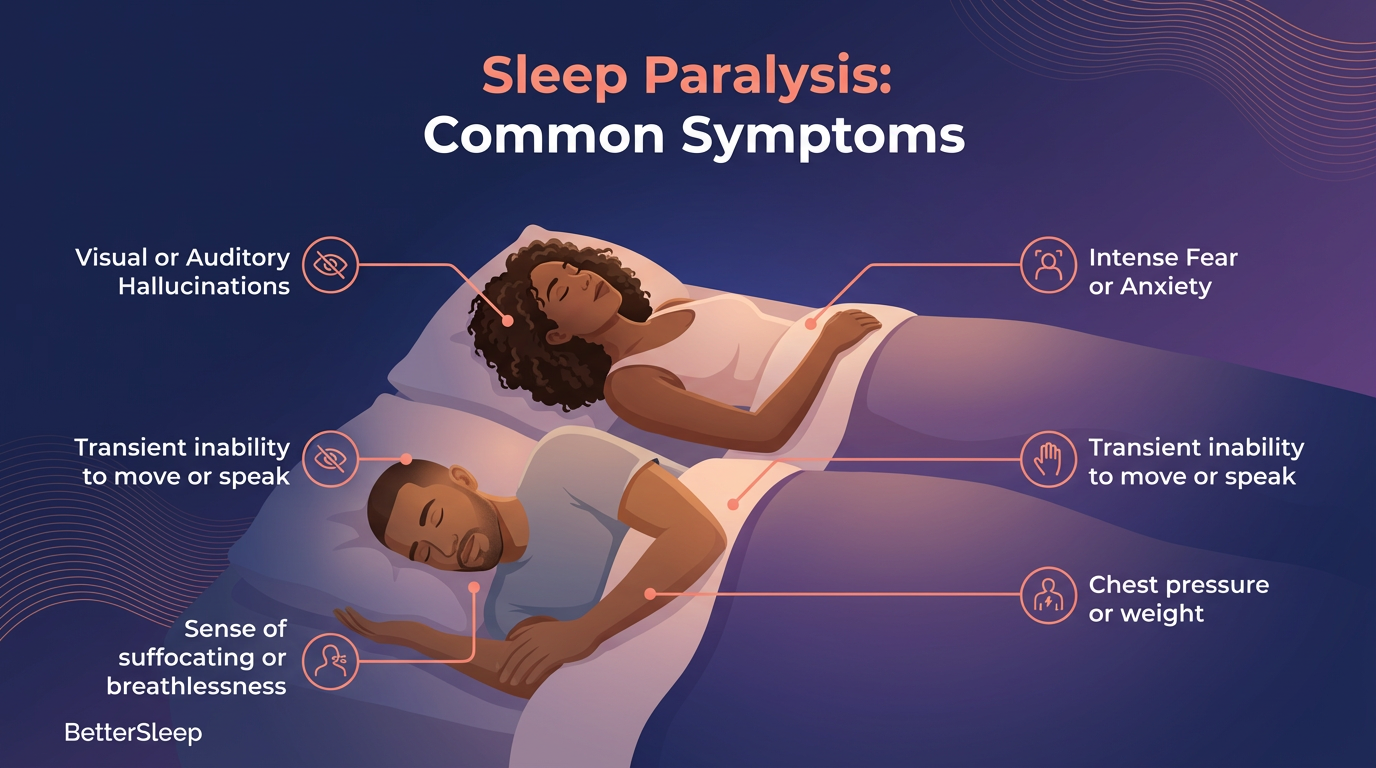
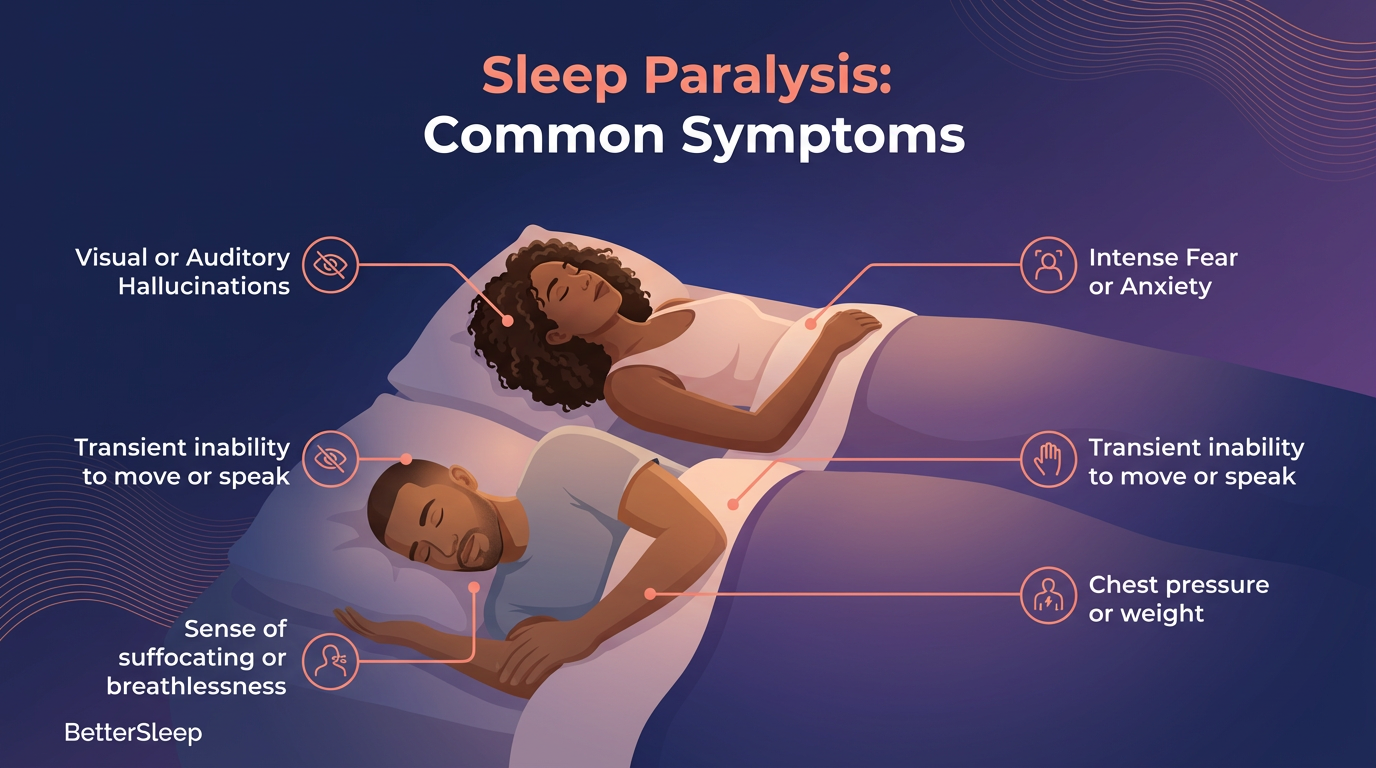
Sleep paralysis is one of those experiences that feels impossible to describe until it happens to you. You wake up, your mind is clear, and your surroundings feel familiar—but your body won’t move. Some people feel a crushing weight on their chest. Others sense someone in the room. A few even feel as if they’re floating, spinning, or sinking through the bed. The details differ, but the sense of being trapped inside your own body is nearly universal.
What makes these moments so vivid is that your body is still in REM sleep while your mind is awake. You’re aware, yet still partially dreaming. The result is a mix of real sensations, dream imagery, and emotions so intense they can feel life-threatening—even though they’re not.
The range of sensations
Sleep paralysis tends to follow a predictable pattern. Awareness arrives first, followed by the realization that you can’t move or speak. Breathing may feel shallow or tight, not because your airway is blocked, but because your chest muscles are still in their dream-state relaxation. A sense of pressure or heaviness often accompanies this, especially around the chest or throat. For some, it feels like suffocating; for others, it’s as if being held down by an unseen force.
Despite how frightening these sensations can be, they pose no physical danger. Heart rate and oxygen levels remain normal throughout an episode. Knowing this can help calm the panic when it happens.
The “sleep paralysis demon”
One of the most striking parts of sleep paralysis is the hallucination—imagery so realistic that people around the world have built folklore to explain it. Studies show that about 75 percent of episodes include vivid perceptual experiences that feel entirely external. Scientists divide these into three main types:
- Intruder hallucinations – the sense that someone or something threatening is in the room. You might hear footsteps, whispers, or see a shadowy figure near the bed.
- Incubus hallucinations – sensations of pressure on the chest, difficulty breathing, or a feeling that a being is sitting or pressing on you. These are among the oldest cultural descriptions of sleep paralysis, appearing in myths from Europe, Asia, and Africa.
- Vestibular-motor hallucinations – sensations of movement, such as floating, flying, spinning, or an out-of-body experience. People often describe watching themselves from above or drifting beyond their physical form.
All three stem from the same process: the brain’s REM dream activity leaking into wakefulness, creating experiences that feel absolutely real.
The brain’s role in hallucinations
Neuroscientists Baland Jalal and V.S. Ramachandran have shown that during sleep paralysis, the brain’s “dream generator” remains active while sensory and motor areas regain wakefulness. The result is a hybrid state where dream images are projected onto the waking environment.
That’s why the shapes, voices, or sensations you perceive feel so real—they’re powered by the same neural systems that create dreams, only now you’re conscious of them.
Dr. J. Allan Hobson of Harvard Medical School, had said:
“The hallucinations experienced during sleep paralysis result from a unique state where the brain’s dream-generating mechanisms remain active while consciousness is preserved. This creates a hybrid state that can produce vivid, often frightening perceptual experiences that feel completely real.”
Understanding that these visions are neurological—not supernatural—can be deeply grounding. Once you know what’s happening, the mystery loses its edge.
The emotional impact
Even with that knowledge, an episode can stir up intense emotions. Fear surges first, fueled by adrenaline and immobility. Some people describe a sense of doom; others feel sadness or anger afterward. It’s completely normal to feel shaken or exhausted once it passes.
Over time, though, many people notice that reassurance works better than resistance. A calm internal reminder—this will pass, my body is safe—can shorten the episode and reduce the frequency of future ones.
BetterSleep’s symptom tracking feature helps users record the sensations, timing, and duration of each episode. As you track your episodes, patterns often emerge: a stressful week at work, inconsistent sleep, maybe a late coffee. Seeing those links makes it easier to address the root causes.
Culture and interpretation
Across the world, these sensations have been given different names and explanations. In Cambodia, the experience is described as “the ghost pushes you down.” In Japan, it’s kanashibari, meaning “bound in metal.” In Newfoundland, it’s “the Old Hag.” And in parts of West Africa, people speak of a spirit or demon pressing on the chest.
Anthropologist Devon Hinton and colleagues found that how someone interprets the event shapes how distressing it feels. When it’s framed as a spiritual attack, fear skyrockets and episodes can recur more frequently. But when people learn that it’s simply a physiological event—an overlap between REM sleep and wakefulness—the fear softens, and episodes often fade.
Duration and frequency
Episodes usually last from a few seconds to two minutes, though they can feel far longer in the moment. Some people experience one or two in their entire life; others go through clusters during times of stress or exhaustion. Keeping a consistent sleep schedule and finding reliable ways to wind down before bed—breathing exercises, meditation, or journaling—can help reduce frequency dramatically.
Safety and Medical Facts: Is Sleep Paralysis Dangerous?


If you’ve ever woken up frozen in place, heart pounding, it’s natural to wonder if something serious is happening. The immobility, pressure, and vivid imagery can make sleep paralysis feel life-threatening—but it isn’t.
What’s actually happening
During normal REM sleep, your brain temporarily relaxes your muscles to keep you from acting out dreams. Sleep paralysis occurs when awareness returns before that safety mechanism switches off. For a few seconds, your mind is awake while your body remains in that dream-state stillness. The experience is startling but medically harmless.
Physiologically, nothing dangerous is taking place. Breathing continues, oxygen levels stay normal, and the body quickly resumes full movement. The fear itself is what makes the event feel extreme. Once you understand that, the anxiety tends to fade.
It’s not a sign of a larger illness
Many people worry that sleep paralysis means something is wrong with their brain or heart. In reality, it’s a common, benign parasomnia. It’s distinct from conditions like seizures, panic attacks, or cardiac events—none of which follow the same predictable pattern of immobility paired with full awareness.
That said, frequent or severe episodes can overlap with other sleep disorders such as narcolepsy or sleep apnea. If you often wake up gasping or feel excessively tired during the day, a professional evaluation can rule those out. But for most people, sleep paralysis exists on its own and poses no medical threat.
Debunking common fears
“Can sleep paralysis kill you?”
No. There’s no evidence that it can stop your breathing or your heart. The paralysis only affects voluntary muscles, not those controlling essential functions.
“What if I stop breathing?”
You won’t. The breathing sensations during an episode feel strange because chest and throat muscles are relaxed, but airflow continues normally. Reminding yourself of this can help ease panic in the moment.
“Can I get stuck like that?”
No. Every episode ends on its own, usually within seconds or minutes. You can’t remain paralyzed indefinitely, and no one has ever been medically “trapped” in this state.
“Does it mean I’m going crazy?”
Absolutely not. Sleep paralysis doesn’t indicate psychosis or hallucination disorders. It’s purely a physiological overlap between REM sleep and wakefulness—something the brain occasionally does under stress or disrupted sleep patterns.
“Is this a supernatural experience?”
In many cultures, it’s been described as possession, demonic attack, or spiritual visitation. Today we know these interpretations stem from how vivid REM hallucinations can feel. Modern neuroscience shows they’re dream imagery appearing in the waking state, not external entities.
Hear it from Dr. Emmanuel Mignot, a professor at Stanford Sleep Medicine Center:
“Sleep paralysis represents a fascinating window into the complexity of REM sleep regulation. While episodes can be distressing, they actually demonstrate the sophisticated neural mechanisms that normally protect us during dreaming sleep by preventing physical movement.”
When to see a doctor
Although sleep paralysis itself isn’t harmful, it can sometimes signal deeper sleep disruption. Consider talking to a healthcare professional if:
- Episodes occur weekly or multiple times per night
- You experience intense anxiety or dread around bedtime
- You also have symptoms of another sleep disorder, such as loud snoring, choking, or sudden daytime sleep attacks
- Sleep paralysis causes ongoing insomnia, exhaustion, or fear of sleep
A sleep specialist may recommend a study to track brain and muscle activity overnight. Treatments often focus on improving sleep hygiene—regular schedules, reduced caffeine and alcohol, and stress management—rather than medication.
Finding reassurance and reliable help
The most effective antidote to fear is knowledge. Understanding that sleep paralysis is a harmless glitch in REM transition—not a medical or supernatural threat—helps you regain control over the experience. For guidance, sleep tips, and personalized strategies to improve rest, explore BetterSleep’s blog.
At its core, sleep paralysis is less a medical emergency than a reminder of how intricate—and well-designed—your sleep system truly is. Knowing that transforms those seconds of fear into a fleeting curiosity, one that ends not in danger but in understanding.
Causes and Risk Factors: Why Sleep Paralysis Happens
Sleep paralysis may seem random the first time it happens, but research shows it’s often linked to clear biological, environmental, and emotional patterns. Understanding those patterns can make the experience feel less mysterious and much more manageable.
How sleep paralysis starts
At its core, sleep paralysis is a timing issue. During REM sleep, your brain paralyzes most muscles so you don’t act out your dreams. The problem arises when awareness returns before that paralysis fades. The mind wakes up while the body is still “asleep.”
Why that happens in some people and not others depends on a mix of factors—genetics, sleep quality, mental health, lifestyle habits, and even sleeping position.
Genetic and biological factors
There’s some evidence that susceptibility can run in families. Twin studies suggest a heritable component, possibly linked to genes that regulate REM sleep transitions. If a parent or sibling experiences sleep paralysis, your likelihood increases.
Brain chemistry also plays a role. Neurotransmitters like serotonin and norepinephrine help control the sleep-wake cycle. Small differences in how these systems reset between stages may leave certain people more prone to REM “carryover” into wakefulness.
Physiologically, this isn’t a malfunction—it’s simply a brief delay in the body’s natural safety process. Think of it as a door closing just a beat too late.
Environmental and lifestyle triggers
Certain habits and conditions make that timing misfire more likely. The most common include:
- Irregular sleep schedules – working shifts, studying late, or changing time zones can disrupt the body’s circadian rhythm.
- Sleep deprivation – missing even a few hours of rest increases REM pressure, which can intensify episodes once you finally sleep.
- Sleeping on your back – this position may restrict airflow slightly and is frequently reported by people who experience sleep paralysis.
- Stress and anxiety – high stress levels are strongly correlated with episodes, likely because of heightened arousal and fragmented sleep.
- Substance use – alcohol, caffeine, and certain medications (especially antidepressants that affect REM) can alter normal sleep cycles.
Each factor can push the REM system slightly off balance. Combined, they create the perfect storm.
Sleep disorders and comorbidities
Sleep paralysis often overlaps with other sleep disruptions. The most commonly associated are:
- Narcolepsy – a neurological disorder involving sudden sleep attacks and REM intrusion into wakefulness. Many people with narcolepsy experience sleep paralysis as part of their condition.
- Insomnia – fragmented or poor-quality sleep increases REM rebound and the likelihood of partial awakenings.
- Sleep apnea – pauses in breathing can jolt the brain awake repeatedly, creating the same fragmented transitions that lead to paralysis.
- PTSD and anxiety disorders – hypervigilance and nighttime arousal make it harder for the brain to move smoothly between sleep stages.
A systematic review found that individuals with these conditions were significantly more likely to report sleep paralysis than the general population.
Age, gender, and demographics
Sleep paralysis can happen at any age, but it’s most common in teens and young adults—roughly ages 17 to 30—when sleep patterns tend to be irregular and stress levels high. It can occur in older adults too, often tied to medical conditions or disrupted routines.
Some studies show a slightly higher prevalence among women, possibly related to hormonal factors or higher reported rates of insomnia and anxiety. Ethnicity and cultural background may influence how people interpret the event, but biologically, the mechanism is the same across populations.
Emotional and psychological patterns
Emotions play a powerful role in sleep. Anxiety, trauma, or chronic stress keep the nervous system on alert, even during rest. That “on edge” state makes it harder for the brain to transition smoothly in and out of REM.
Researchers describe a feedback loop: the more distress an episode causes, the more likely you are to fear sleep, which increases arousal and perpetuates the problem. Addressing anxiety can therefore be one of the most effective ways to reduce frequency.
If your episodes often follow periods of worry, racing thoughts, or burnout, that’s not coincidence—it’s physiology. Calming the mind helps the body recalibrate.
BetterSleep offers many ways to support that calm, from guided breathing, mindfulness exercises to relaxation techniques clinically shown to lower nighttime arousal. Incorporating these strategies can make sleep paralysis far less likely.
Recognizing your own triggers
Not everyone’s pattern looks the same. Some people notice episodes after pulling all-nighters; others only when they nap on their back. Keeping a brief sleep journal or using a symptom-tracking app can help pinpoint what’s contributing to yours.
Over time, those small data points reveal actionable insights: maybe a stressful week aligns with shorter sleep times, or maybe caffeine after 3 p.m. makes nights rougher. Once you identify your triggers, you can take back control. Simple adjustments—consistent bedtimes, winding down before bed, practicing relaxation—often reduce or eliminate episodes altogether.
Knowing why sleep paralysis happens is only half the story—the other half is learning how to respond to it. Once you recognize the patterns behind your episodes, you can start building habits that retrain your body to move smoothly between sleep and wakefulness.
Immediate Relief and Prevention Strategies
Sleep paralysis may not be dangerous, but in the moment, it can feel overwhelming. The good news is that there are reliable ways to break an episode as it happens—and even better ways to stop them from coming back. By combining quick-response tactics with long-term habits that strengthen sleep quality, most people see dramatic improvement.
How to stop a sleep paralysis episode in progress
1. Focus on your breath.
Remind yourself that you’re breathing normally, even if it feels tight or shallow. Slow, steady breaths can reduce panic and help your body transition out of REM faster.
2. Move small muscles first.
Try wiggling a single finger, toe, or your tongue. Movement in smaller muscles often triggers the full body to “wake up.” Some people find repeatedly trying to blink or roll their eyes breaks the paralysis.
3. Shift your focus, not your effort.
Rather than struggling to move, redirect your attention to something calming—counting, reciting lyrics, or visualizing a relaxing place. This engages waking neural networks and gently pulls the body out of the REM state.
4. Regulate fear.
Remember: the sensations are temporary and harmless. Mentally labeling them (“this is sleep paralysis”) helps reduce the brain’s threat response, shortening the episode.
5. Keep light nearby.
If episodes are frequent, consider a small bedside light or smart bulb you can trigger with a voice command once movement returns. Immediate light helps re-orient your brain to wakefulness.
These techniques may sound simple, but practiced regularly, they can make episodes shorter and less intense.
Building habits that prevent recurrence
Long-term prevention focuses on stabilizing your sleep cycle and lowering nighttime stress. The most effective strategies are consistent, not complicated.
1. Maintain a steady sleep schedule.
Go to bed and wake up at roughly the same time—even on weekends. Consistency trains your circadian rhythm to expect sleep and reduces fragmented REM transitions.
2. Prioritize full sleep.
Adults need 7–9 hours nightly. Skipping sleep or staying up late builds REM pressure, which increases the likelihood of sleep paralysis once you finally rest.
3. Sleep on your side.
Back-sleeping is the position most associated with episodes. Try using a body pillow or positioning cushion to encourage side sleeping.
4. Limit stimulants and alcohol.
Caffeine after mid-afternoon or alcohol close to bedtime can both disrupt REM balance. Moderate use and earlier timing go a long way.
5. Create a relaxing wind-down routine.
Dim lights, stretch lightly, read, or listen to soothing audio before bed. Pairing relaxation with bedtime teaches your body that rest—not adrenaline—comes next.
Dr. Michael Grandner of the University of Arizona summarizes it well:
"Effective sleep paralysis management requires a comprehensive approach addressing sleep hygiene, stress reduction, and underlying sleep disorders. In my experience, patients who implement consistent sleep schedules and stress management techniques see significant improvement in episode frequency and intensity."
Optimizing your sleep environment
Your sleep environment matters just as much as your schedule. A calm, comfortable space reduces micro-awakenings—the small disruptions that can trigger sleep paralysis.
- Keep it dark, cool, and quiet. Aim for 60–67°F (15–19°C) and eliminate stray light or noise.
- Upgrade bedding. Comfortable, breathable fabrics prevent tossing and turning that fragments sleep.
- Reserve your bed for rest. Avoid scrolling or working in bed—train your brain to associate it exclusively with sleep.
- Use scent or sound cues. Calming sounds and essential oils can signal bedtime in a predictable, comforting way.
For more guidance on shaping the perfect environment, BetterSleep can help you improve your sleep hygiene practices plus optimize your sleep environment for better rest and recovery.
Managing stress and nighttime anxiety
Stress is one of the strongest triggers for sleep paralysis. Learning to calm the body before bed reduces the risk dramatically. Techniques that lower heart rate and muscle tension can interrupt the physiological chain that leads to REM misfires.
Try these before bed or anytime stress builds:
- Guided breathing. Practice 4-7-8 breathing: inhale for 4 seconds, hold for 7, exhale for 8.
- Gentle stretching. Ease tension with a few slow shoulder rolls or a seated forward fold. Releasing tightness signals to your body that it’s time to rest.
- Progressive muscle relaxation. Tense and release each muscle group from head to toe to drain physical stress.
- Mindfulness meditation. Spend a few minutes observing your thoughts without judgment, letting the mind settle naturally.
- Sound or scent cues. Play a calming playlist or diffuse lavender or chamomile essential oils. Over time, your brain begins to associate those cues with relaxation.
- Journaling. Write down worries or to-dos before bed to keep them from resurfacing overnight.
BetterSleep’s in-app library includes dozens of guided relaxation techniques and stress management tools designed specifically to reduce nighttime arousal. Regular use can help train your body to enter sleep peacefully—and stay there.
Addressing underlying sleep disorders
If lifestyle changes aren’t enough, persistent sleep paralysis might be linked to another sleep condition, such as narcolepsy, sleep apnea, or chronic insomnia. These conditions fragment sleep and disrupt REM cycles. Professional evaluation through a sleep clinic or polysomnography can pinpoint these issues. Treatment might involve airway therapy for apnea, medication adjustment, or cognitive behavioral therapy for insomnia (CBT-I).
You don’t need to face these challenges alone. BetterSleep’s sleep-tracking insights and educational articles can help you spot patterns that might warrant medical follow-up—and guide you toward conversations with qualified professionals if needed.
Finding your rhythm again
Breaking the cycle of sleep paralysis isn’t about perfection—it’s about consistency. When you give your body enough rest, manage stress, and make your environment genuinely restful, your brain relearns how to flow through every sleep stage smoothly. Episodes become shorter, then rarer, then—for lots of people—disappear altogether.
And on the rare nights when they return, you’ll know exactly what to do: breathe, wait, and trust your body to finish what it started.
Treatment Options and Professional Help
For most people, simply understanding what’s happening and improving sleep habits is enough to keep sleep paralysis from returning. But if episodes are frequent, frightening, or interfere with rest, professional support can make a big difference. Treatment typically combines education, behavioral therapy, and—when needed—medical evaluation.
Education comes first
The foundation of treatment is knowledge. Once you understand that sleep paralysis is a harmless REM-related event, your fear response changes. Many people see improvement simply by learning what triggers their episodes and how to respond calmly.
Dr. Brian Sharpless, a clinical psychologist at Washington State University who has studied the condition extensively, explains:
“In my clinical practice, I’ve found that education and cognitive behavioral techniques are often the most effective first-line treatments for recurrent sleep paralysis. When patients understand what’s happening to their brain and body during episodes, they develop better coping strategies and experience reduced frequency.”
BetterSleep’s blogs and sleep-tracking features support this first step—helping you recognize patterns, understand triggers, and feel more in control of your nights.
Cognitive and behavioral strategies
When education alone isn’t enough, many therapists use cognitive behavioral therapy (CBT) to address the fear and anticipation surrounding sleep paralysis. Through CBT, you can:
- Reframe catastrophic thoughts (“I’m dying”) into realistic ones (“My body will move again in a few seconds”).
- Build confidence about going to bed instead of avoiding sleep.
- Practice relaxation and grounding skills for when episodes happen.
CBT can also reduce broader stress and anxiety—two of the strongest predictors of sleep paralysis. Even a few sessions focused on sleep-related worries can make a measurable difference.
Medication as a secondary option
Medication isn’t necessary for most people, but in persistent or severe cases, doctors may consider it to stabilize REM sleep. Common approaches include:
- Antidepressants (SSRIs or tricyclics): reduce the amount of REM sleep and limit paralysis episodes.
- Short-term sedatives: occasionally prescribed to break cycles of insomnia or anxiety that keep sleep fragmented.
These are always prescribed by a healthcare professional and monitored carefully for side effects. Behavioral methods generally remain the cornerstone of treatment.
Evaluating related sleep disorders
Sometimes, sleep paralysis occurs alongside other sleep issues. If you experience loud snoring, gasping for air, excessive daytime sleepiness, or sudden loss of muscle control, a sleep specialist can test for conditions like narcolepsy, sleep apnea, or chronic insomnia.
An overnight study (polysomnography) or at-home test can identify whether another disorder is fragmenting your REM cycles. Treating that underlying issue—through airway therapy, medication adjustments, or structured behavioral sleep therapy—often resolves the paralysis, too.
What to expect from treatment
Sleep paralysis is highly responsive to lifestyle and behavioral changes. Most people who work with a clinician or consistently apply CBT and relaxation techniques report major improvement within one to two months. Episodes may become less frequent, shorter, and far less frightening.
Even if they return occasionally, they’re easier to manage because now you know what’s happening and how to ride it out calmly.
A realistic, supportive approach
Treatment doesn’t mean medicalizing your sleep—it’s about giving you tools to understand it. With consistent sleep hygiene, a few mental-health strategies, and occasional professional input, most people regain confidence in their nights.
BetterSleep’s role is to support that journey: offering credible education, mindfulness tools, and science-based guidance so you can apply what you learn in therapy—or on your own—with confidence.
Lifestyle and Self-Care Strategies
Once you understand what sleep paralysis is and how to manage it, the next step is building habits that keep your sleep steady long-term. The goal isn’t to live in fear of another episode—it’s to create a lifestyle that supports deep, restorative rest so episodes fade into the background of a healthy routine.
Prioritizing the basics
Good sleep starts with good foundations. Regular exercise, balanced nutrition, and hydration all play powerful roles in how your body regulates sleep cycles.
- Move often. Moderate daily activity—like walking, cycling, or yoga—helps reduce stress hormones and promotes stable REM sleep. Just avoid intense workouts right before bed.
- Eat for steady energy. Heavy meals or high-sugar snacks late at night can delay sleep onset. Aim for balanced meals with complex carbs, lean proteins, and magnesium-rich foods that naturally support muscle relaxation.
- Stay hydrated (but not right before bed). Dehydration can disrupt sleep quality, but drinking too much water close to bedtime can have the same effect.
Consistency across these basics often does more for sleep paralysis than any single intervention.
Mind-body balance
Because stress and anxiety are common triggers, building calm into your day matters as much as how you end it. Try micro-moments of relaxation: a short breathing exercise between meetings, a mindful walk, or jotting down what’s on your mind before bed.
If racing thoughts keep you up, techniques like guided imagery, gratitude journaling, or gentle meditation can retrain the brain to associate bedtime with safety and release.
Technology that helps (instead of hinders)
Technology is often blamed for poor sleep—but used intentionally, it can be a powerful ally. Sleep apps, smart devices, and wearables can all help you understand your patterns and fine-tune your habits.
BetterSleep provides ongoing support through sleep tracking, relaxation techniques, and educational resources designed specifically for individuals managing sleep disorders. Our advanced sleep tracking features for pattern recognition can help you see what’s working, spot triggers, and celebrate progress over time.
When using tech, set healthy boundaries: switch your phone to night mode, dim your screen, and avoid endless scrolling before bed. The goal is to use tools that guide, not overstimulate.
Community and support systems
Sleep issues can feel isolating, especially when episodes are rare but intense. Finding others who understand can make the experience less frightening. Online communities and educational groups offer reassurance that you’re not alone.
If you live with a partner or family member, explaining what sleep paralysis looks like can also help. They’ll know what’s happening if you wake up frozen and can remind you that it’s temporary and safe.
Long-term management and mindset
Ultimately, self-care for sleep paralysis is about shifting from reaction to prevention. Instead of focusing on the episodes themselves, focus on everything that makes quality sleep easier: steady routines, emotional regulation, and a supportive environment.
When you care for your mind and body throughout the day, your nights naturally follow suit. Over time, the episodes that once felt terrifying become rare reminders of how resilient—and adaptable—your sleep system truly is.
Frequently Asked Questions About Sleep Paralysis
How long does sleep paralysis typically last?
Episodes usually last anywhere from a few seconds to two minutes—though they can feel much longer. The exact length depends on how quickly your brain transitions out of REM sleep and how calm you can stay in the moment. Panic tends to extend the experience, while slow breathing and mental grounding help it end faster. Even during longer episodes, the body remains safe and breathing normally, and movement always returns on its own.
Can children experience sleep paralysis?
Yes, although it’s less common in young children. Sleep paralysis can begin in adolescence, often around puberty when sleep schedules become irregular and stress increases. Younger kids might experience similar sensations but lack the language to describe them. If a child reports feeling “stuck” or “unable to move” while waking, reassure them that it’s not dangerous and encourage regular sleep routines. Consistent bedtimes, calming activities, and reduced screen time can help minimize episodes.
Is sleep paralysis hereditary or genetic?
Genetics can play a role, but it’s not a simple inheritance pattern. Studies suggest that people with a family history of sleep paralysis may have a higher likelihood of experiencing it themselves, likely due to shared traits that influence REM regulation and sleep stability. However, environmental and lifestyle factors—like stress, caffeine, or disrupted sleep—are often just as important. If it runs in your family, consistent sleep habits are your best form of prevention.
Can sleep paralysis be completely cured or prevented?
There isn’t a guaranteed “cure,” but for most people, sleep paralysis is completely manageable. With consistent sleep schedules, stress reduction, and healthy nighttime habits, episodes often fade or disappear altogether. Clinical studies show significant improvement for those who address both sleep hygiene and anxiety triggers. In rare cases where episodes persist, therapy or medication can help stabilize REM cycles. The key is management, not perfection—progress comes from small, steady adjustments.
What should I do if my partner experiences sleep paralysis?
If your partner wakes up unable to move or speak, the most helpful thing you can do is stay calm and reassure them. Gently saying their name, turning on a light, or lightly touching their arm can help ground them once movement returns. Avoid shaking or startling them; the paralysis will end naturally. Later, encourage open conversation about the episode and consider shared bedtime habits—like winding down together or sticking to a consistent sleep schedule.
Are there any medications specifically for sleep paralysis?
There are no medications made solely for sleep paralysis, but doctors sometimes prescribe drugs that regulate REM sleep when episodes are frequent or severe. These can include certain antidepressants (SSRIs or tricyclics) that reduce the proportion of REM sleep. Medication is typically reserved for chronic cases or those linked to other conditions like narcolepsy. Most people improve without it, using behavioral and lifestyle strategies instead. Always discuss options with a qualified healthcare provider before starting any treatment.
How is sleep paralysis different from other sleep disorders?
Unlike nightmares or night terrors, sleep paralysis occurs during the transition between REM sleep and wakefulness, when consciousness returns before movement does. Nightmares happen during REM but include vivid dreams that cause awakening, while night terrors occur during deep non-REM sleep and involve confusion or screaming without full awareness. Sleep paralysis, by contrast, leaves you fully aware but physically still. Understanding this difference helps demystify what’s happening and distinguishes it from other parasomnias.
When should I see a doctor about sleep paralysis?
Occasional episodes don’t usually require medical attention. However, it’s a good idea to consult a healthcare provider if paralysis happens more than once a week, causes severe anxiety, or leads to chronic insomnia. You should also seek evaluation if you experience additional symptoms—such as gasping for air, excessive daytime sleepiness, or sudden loss of muscle control—as these may point to another sleep disorder. A sleep specialist can help identify triggers and recommend tailored treatment.
Sleep paralysis can be unsettling, but understanding it gives you back your sense of control. With consistent sleep habits, stress-reduction tools, and a calm mindset, most people find that their nights become peaceful again. For extra support, the BetterSleep app can help you track patterns, relax before bed, and fall asleep faster with guided breathing, meditations, and soothing sounds. Download it today and start turning restless nights into sweet dreams.
Resources:
- https://www.pbs.org/wgbh/nova/article/the-nightmare-of-sleep-paralysis/
- https://my.clevelandclinic.org/health/diseases/21974-sleep-paralysis
- https://www.nature.com/articles/nrn915
- https://my.clevelandclinic.org/health/diseases/12133-parasomnias--disruptive-sleep-disorders
- https://aasm.org/clinical-resources/international-classification-sleep-disorders/
- https://www.mountsinai.org/health-library/diseases-conditions/isolated-sleep-paralysis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6909245/
- https://sleepeducation.org/what-you-never-knew-about-sleep-paralysis/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4950339/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10218966/
- https://yokai.com/kanashibari/?srsltid=AfmBOoriBbozgblqmr9LFatUhjIMsA2gCmxBsewRy117qcnw2FPtUvMl
- https://www.health.harvard.edu/diseases-and-conditions/sleep-paralysis-causes-symptoms-and-treatments
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4141319/
- https://www.sleepfoundation.org/parasomnias/sleep-demon
- https://pubmed.ncbi.nlm.nih.gov/28293186/
- https://health.umms.org/2022/08/26/sleep-paralysis/
- https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep
- https://www.sleepfoundation.org/parasomnias/sleep-paralysis
- https://my.clevelandclinic.org/health/diseases/21974-sleep-paralysis
- https://my.clevelandclinic.org/health/diagnostics/12131-sleep-study-polysomnography
- https://pubmed.ncbi.nlm.nih.gov/28735779/
- https://my.clevelandclinic.org/health/articles/22572-serotonin
- https://my.clevelandclinic.org/health/articles/22610-norepinephrine-noradrenaline
- https://www.nhlbi.nih.gov/health/sleep/sleep-wake-cycle
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3156892/
- https://pubmed.ncbi.nlm.nih.gov/10214743/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6879567/
- https://health.clevelandclinic.org/4-7-8-breathing
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8272667/
- https://www.mayoclinic.org/tests-procedures/polysomnography/about/pac-20394877
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10002474/
- https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
- https://www.aafp.org/pubs/afp/issues/2011/1101/od1.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4958367/
- https://pubmed.ncbi.nlm.nih.gov/19496997/